Why This Strategy Matters
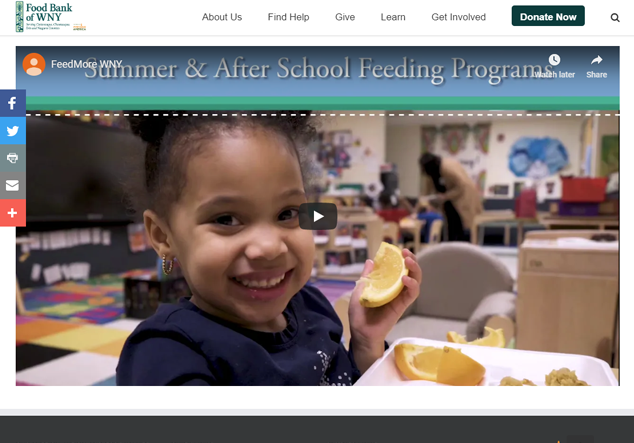
Nearly 95,000 residents in the region, including 21,600 children, live in neighborhoods designated by the USDA as "food deserts" where healthy food access is limited and food insecurity is high. Nearly half of these individuals live in or near poverty, so being able to afford food is a constant concern for many. Not having a car adds another obstacle, and nearly a quarter (22%) of households in food deserts do not own a vehicle. Overcoming these barriers to make healthy food more affordable and accessible is critical. A healthy diet can help prevent obesity and curb related health conditions like diabetes, heart disease, and hypertension. Moreover, many strategies to improve healthy food access, like community gardening, also benefit physical and mental health.